Over the past year, I’ve centered my work around women’s health and a simple but powerful idea that came from that: no one should have to figure out how to navigate pregnancy care on their own. Especially not while working full-time.
It’s a belief that’s shaped every important conversation I’ve had with HR leaders, every piece of advice I’ve offered to health and benefits teams, how I’ve supported innovative founders in the space, and most recently, what I shared in “The System Wasn’t Built for Us.”
Despite all the talk about women’s health in the workplace, pregnancy still functions as a stress test, not just for the employee, but for the systems meant to support them. While the burden is particularly heavy for women navigating pregnancy, it also underscores long-standing inequities in care for women in many situations, especially women of color who routinely face greater barriers to access. What should be a guided, supported care experience often turns into a mess of plan confusion, last-minute provider changes, surprise costs, and far too many unanswered questions.
This isn’t just a breakdown in process. It’s a design problem. The way we’ve structured healthcare and benefits doesn’t reflect how people actually move through pregnancy or any real-life care journey, for that matter.
And yet, this moment offers a real opening for HR leaders like myself. Pregnancy is one of the few times when employees are already deeply engaged. They’re searching for answers, trying to prepare, doing their best to make the right decisions. That’s the window when support has the most impact.
This piece is a call to action for HR and benefits leaders: don’t wait. Step in earlier. Support smarter. And stop treating navigation like a side feature. If we’re serious about improving outcomes, retaining talent, and building real equity into our systems, we have to show up when it matters most and for those who truly need the support.
The System Was Not Built With Women in Mind
Pregnancy is not a single event. It’s part of a much longer journey that includes preconception, frequent doctor visits, postpartum recovery, and long-term health. But the systems meant to support that journey (healthcare, insurance, and workplace benefits) were rarely designed with that full picture in mind.
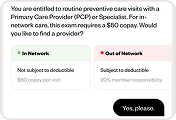
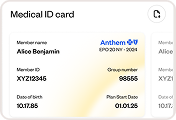
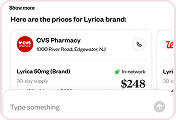
Too often, those structures fall apart right when people need them most. Narrow networks, confusing language surrounding benefits coverage, unclear billing, and a lack of price transparency make it hard to plan ahead. For many employees, staying with a trusted OB-GYN through a plan change or job transition is nearly impossible. Even with high-quality, employer-sponsored insurance, people can find themselves mid-pregnancy without a provider or a straight answer.
And once the baby is born, the focus shifts quickly. Newborns get regular checkups scheduled at a regular cadence, and rightly so. But birthing parents? They are discharged from the hospital (sometimes before their newborn) and might go six weeks without a single follow-up. That’s not a mere missed appointment; it’s a sign of a system that puts maternal health on the back burner at one of the most critical points in care.
For employers, this is a gap in responsibility. If your benefits don’t reflect what people actually go through during and after pregnancy, they aren’t working. Equitable care means acknowledging the system wasn’t built for women, and then doing the real work to rebuild it with their experiences front and center.
The Burden of Advocacy Should Not Fall on Pregnant Employees
In the moments that matter most, our system too often puts the burden of navigation on the people who are the least equipped, or the least supported, to carry it. For pregnant employees, that weight shows up in all kinds of ways. They’re scrambling to find an in-network OB-GYN. They’re trying to figure out coverage in the middle of an appointment. Sometimes, they lose their provider altogether because of a job change or open enrollment.
These aren’t rare cases. They’re built into the system. And without real, proactive support, they pile up right when employees should be focusing on their health and preparing for a growing family, not battling paperwork or guessing what’s covered. The result? Employees become the default administrators for their own care. They’re calling around for answers, reading through confusing benefits guides, and realizing too late what isn’t covered.
This is where the navigation we assume is intertwined with the benefits we offer needs to evolve. It shouldn’t be a static resource that people may find when they’re in a crisis. It has to be a living, responsive strategy that guides and advocates for people in real time. And that’s where employer insight becomes critical.
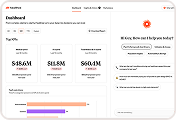
In Healthee’s recent Benefits Divide report, maternity-related searches consistently ranked among the highest across employee populations.1 This is a signal. Employees are telling us where and when they need help. They’re attempting to solve this healthcare crisis on their own and are willing to step out of their own comfort zone to do it. They’re open to asking questions, sharing information, and trying new things to get what they need. This is our chance to help them in a way that provides the safest and lowest-cost outcomes, which benefits us all.
The question for HR leaders right now isn’t whether support is needed. It’s whether your system can actually provide it when they ask for help. In too many cases, because we are all relying on the system as it’s currently built, the answer is still, “not really.”
It doesn’t always require a new benefit. And it definitely doesn’t have to cost more. We can make better use of what’s already in place. Tools like Healthee can take the intent behind those searches and turn it into guided, personalized support in those moments when employees are already leaning in.
Equity Must Be Central to Maternal Care Navigation
Maternal health disparities in the U.S. aren’t theoretical. They’re measurable, preventable, and still happening every day. According to the Centers for Disease Control and Prevention, Black women are nearly three times more likely to die from pregnancy-related causes than white women. Native American and Alaska Native women face more than double the risk.2 These outcomes persist regardless of income or education.
Access plays a big role. A 2022 report from the U.S. Government Accountability Office found that nearly 1,200 counties across the country don’t have a hospital with obstetric services or a practicing OB-GYN. That means millions of women of reproductive age live in areas where basic prenatal care is hours away, if it’s available at all.3 These are the same counties where we are hiring our talented remote workers, where we want to see our companies grow, and where we have little to no impact on the ability of the local government or healthcare system to actually do anything significant to improve the health of its population.
These are not edge cases. They’re design failures. And when our benefit strategies ignore them, they allow existing disparities to continue under the surface.
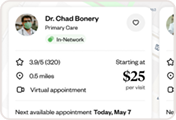
Equity can’t just be something we reference in mission statements. It has to be part of how benefits are built. When someone searches for an OB-GYN, they should find providers who are local, or at minimum, accessible virtually, in-network, available now, and able to deliver care that reflects their lived experience.
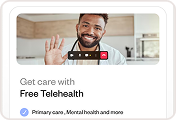
That’s where telehealth becomes not just a convenience, but a critical tool in advancing access. For those living in healthcare deserts, where specialty providers are few and far between, virtual care must be seamlessly integrated into benefits navigation. It should be easy to find, easy to use, and built to bridge the gaps geography and infrastructure create.
If we say we care about equity, then it has to shape how we design and offer our programs. Because if these benefits and navigation tools don’t work for the people most at risk of being left behind, then they don’t work at all.
The New Benefits Strategy
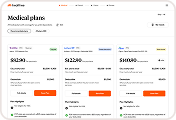
When employers see gaps in their offerings that highlight the lack of support for underserved employees, the default response is often to add another benefit. More logos, more portals, more confusion. But more isn’t always better. And in most cases, it’s not sustainable financially or administratively.
Understanding what’s already available to an employee, what applies to them and their families in the moments that matter, and what to do next once that information is surfaced is the foundation of a successful benefits strategy. That kind of clarity is essential.
As we consider layering on more tools, we should be asking: do employees understand what’s available to them, can they access these benefits when necessary, and do they have the information they need before, after, and during their care? Confident care means understanding your benefits, avoiding unnecessary costs, getting timely care, and feeling supported instead of overwhelmed.
This isn’t just good for employees, it’s smart business. Employers can drive better outcomes and higher engagement without significantly increasing costs. In fact, by streamlining access and eliminating friction, they often save more by helping their workforce do more with the benefits already in place.
And the impact goes beyond just health outcomes. Strong, accessible benefits also play a critical role in employee retention, especially for those growing their families. The memory of being supported during a pivotal life moment often becomes a reason someone chooses to return, even after leaving.
How a company invests in its people, how it delivers on promises and shows it truly cares, shapes the way employees view their workplace. When you get this right, you’re not just saving money or reducing confusion. You’re building the kind of culture where people believe they can thrive, grow, and achieve their personal and professional goals.
That’s the outcome we should be building for. Every single time.
A Call to Action for HR and Benefits Leaders
If we want to improve maternal health outcomes, retain top talent, and actually deliver on equity, we have got to better support employees trying to figure out how to navigate a complex healthcare system on their own.
Design your plans and point solutions with empathy. Pay attention to what people are already searching for. Build benefits for the messy, emotional, real-life moments. And most importantly, remember this: Supporting employees cannot start or stop at open enrollment. It begins every moment someone needs care.
Maternal health is too hard to manage within our current system, but it doesn’t have to be. Let’s change this thing together, one support system at a time.
References:
1. Healthee. (2025). The 2025 Benefits Divide. Retrieved from https://healthee.com/reports/the-2025-benefits-divide/.
2. Centers for Disease Control and Prevention (CDC). (2023). Disparities in Pregnancy-Related Deaths. U.S. Department of Health and Human Services. Retrieved from https://www.cdc.gov/reproductivehealth/maternal-mortality/disparities-pregnancy-related-deaths/index.html
3. U.S. Government Accountability Office (GAO). (2022). Maternal Health: Availability of Hospital-Based Obstetric Services in Rural Areas. GAO-23-105871. Retrieved from https://www.gao.gov/products/gao-23-105871