Open enrollment season can catch employees off guard. Without a strong open enrollment reminder strategy in place, they might miss critical deadlines or rush through decisions that affect their health and finances for the year ahead.
But it doesn’t have to be that way. With the right cadence, clarity, and communication channels, HR teams can turn open enrollment into an opportunity to boost engagement, drive smarter benefits decisions, and reduce last-minute stress.
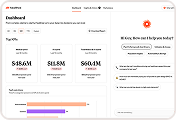
Backed by years of success implementing benefits communications strategies, the team at the Healthee Brief shares our best practices that have led companies to achieve incredible engagement. One Healthee client in the TV and entertainment industry achieved over 70% registration rate with the Healthee platform, leading to successful open enrollment and year-long benefits engagement.
Our guide walks you through how to craft open enrollment reminders that cut through the noise and help your people take confident action.
Why Open Enrollment Reminders Are Essential
Most employees don’t fully understand their health benefits. In fact, only 49% say they feel confident navigating their options, which leads to rushed decisions and long-term dissatisfaction.1
That’s where a well-timed open enrollment reminder comes in. More than just a date check, these messages serve as prompts to act, learn, and engage. They reduce inbox clutter by offering clarity, and they help employees make choices with confidence — not confusion.
And for HR teams? Effective reminders mean fewer last-minute questions, fewer compliance risks, and fewer hours spent answering the same benefit questions over and over.
Best Practices for Sending Open Enrollment Reminders
1. Start Early, and Repeat Thoughtfully
According to SHRM, starting open enrollment communications at least 30 days before the enrollment window opens significantly increases participation.2 Send a series of reminders at strategic intervals: 30 days, 15 days, 7 days, and 1 day before the deadline.
2. Use Multiple Channels
Your reminder shouldn’t get lost in a crowded inbox. Reinforce key messages through Slack, SMS, company intranet, digital signage, and even printed flyers if your workforce isn’t always online. It works, the numbers don’t lie. Harvard Business Review found that multichannel outreach can improve employee engagement by up to 27%.3
3. Make It Personal
Segment your messaging by employee demographics, plan eligibility, or previous elections. Personalized reminders see higher open rates and better decision-making outcomes.
4. Clarify the “Why” and “How”
A subject line like “Reminder: Open Enrollment is here” won’t spark action. Instead, lead with what’s changing, what’s at stake, and how employees can make the right choice. Include how-to videos, enrollment checklists, and plan comparison tools to make the process simple from start to finish.
Need help writing those messages? Check out our open enrollment email template to get plug-and-play copy for every stage of the enrollment journey.
How Healthee Makes Open Enrollment Easier
The best open enrollment reminder doesn’t just nudge employees — it guides them toward better decisions. That’s exactly what Healthee was built to do.
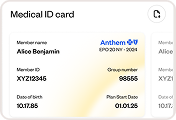
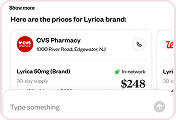
With Healthee, employees don’t have to dig through PDFs or wait on hold. Our AI-powered platform streamlines every step of the enrollment process and answers benefits questions instantly. Here’s how we support your team and your people:
- Personalized reminders: Sent automatically to the right people at the right time
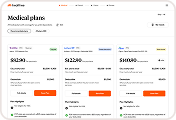
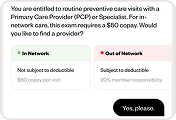
- A plan comparison tool: Helps employees evaluate their options side by side, based on their health needs and usage history
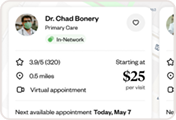
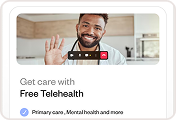
- 24/7 support: Zoe, our conversational AI assistant, who can explain benefits, recommend plans, and help employees find in-network care
- An intuitive interface that simplifies plan selection and reduces confusion during enrollment
With Healthee, open enrollment becomes less about compliance and more about confidence.
Conclusion
A thoughtful open enrollment reminder strategy does more than check a compliance box. It builds trust, reduces stress, and helps employees make confident, informed decisions about their health. When your messages are timely, clear, and personalized, open enrollment stops feeling like a scramble and starts becoming a strategic win, for your people and your HR team.
With Healthee, you can automate reminders, guide plan selection, and give every employee the tools they need to navigate benefits with confidence. It’s time to take the pressure off HR and put better decisions into the hands of your workforce.
References
- BenefitsPro. (2024). Survey: Only Half of Workers Understand Their Benefits. Retrieved from benefitspro.com
- Society for Human Resource Management (SHRM). (2024). Best Practices for Open Enrollment Communication. Retrieved from shrm.org
- Harvard Business Review. (2024). How Multichannel Communication Improves Employee Engagement. Retrieved from hbr.org