Healthcare costs continue to rise globally. And it affects every employee, employer, business, and government alike.
In response, the concept of cost containment in healthcare has emerged as an important strategy to address this escalating financial burden.
So, in this article, we’ll talk about the following:
- What cost containment really is, and how it affects reimbursement rates
- Factors affecting the rising cost of US healthcare spending
- Effective cost containment strategies
- Cost-containment technology that helps employees find the best prices and services for them in just seconds
The current state of healthcare costs in the US health system
Before we jump into cost containment strategies, it’s essential to understand why we have them.
The main reason is the rise in healthcare costs. Here are the numbers:
- Skyrocketing health spending: US healthcare spend was a whopping $4.3 trillion in 2021, at $12,914 per person, and is expected to increase by 5.1% annually to $7.2 trillion by 2031.¹
- Rising health insurance costs: Health insurance costs account for one of the most significant employer expenses in the US, and many companies are expecting it to increase by 5.4%-8.5% in 2024.²
- Higher deductibles: In a Mercer survey, large employers said that they would be requiring employees to pick up 22% of their total health plan premium costs through paycheck deductions in 2024.³
Factors driving healthcare costs
Here are some factors affecting the rising healthcare costs in the United States.
Technological advances in the industry
Rapid technological advancements in healthcare have undeniably improved patient outcomes and treatment options.
However, these innovations may come with a hefty price tag.
Cutting-edge medical technologies, diagnostic tools, and innovative treatments often involve substantial research, development, and implementation costs.
These contribute significantly to the overall expenses in healthcare.
Surging chronic disease cases
The prevalence of chronic diseases, such as heart disease, diabetes, and certain cancers, has surged in recent years.
Treating chronic conditions requires ongoing medical attention, medications, and lifestyle management.
The long-term and often complex nature of these diseases amplifies their financial impact on both individuals and healthcare systems.
Administrative costs for companies
The administrative overheads within the healthcare system are substantial.
Billing, insurance processing, and regulatory compliance demand significant resources and workforce.
Streamlining administrative processes in these areas can play a pivotal role in containing overall healthcare and labor costs.
Pharmacy and specialty drug inflation
Rising costs for specialty drugs — including gene therapies and biologics — are a major driver of employer healthcare spend, with prices continuing to outpace inflation.
These treatments often come with price tags in the six- or seven-figure range, putting pressure on self-funded plans and making pharmacy management an essential part of any cost-control strategy.
Employers are increasingly exploring carve-outs, tiered formularies, and value-based contracting to manage these expenses.
High-cost claimants
A small group of members, often those facing cancer, transplants, or complex chronic conditions, can account for the majority of total healthcare costs.
These individuals typically make up 1% to 5% of a population but can drive 50% or more of total spend.
Advisors and finance teams are turning to analytics tools to identify high-cost claimants earlier, support care navigation, and reduce avoidable emergency or out-of-network costs.
What is cost containment in healthcare?
Cost containment in healthcare is the process of controlling expenses through utilization management, financial plan design (such as MERPs or HRAs), and preventive care technologies to reduce waste without compromising patient outcomes.
It’s about finding a balance where healthcare remains accessible and affordable without compromising its effectiveness or patient well-being.
The urgency of cost containment arises from the exponential growth in healthcare costs, driven by several factors.
Technological advancements, administrative overheads, and the prevalence of chronic diseases all contribute significantly to the mounting costs in healthcare.
Healthcare cost-containment strategies
In response to the mounting healthcare expenses, various strategies have been developed to contain costs while striving to ensure quality care and positive outcomes.
Here are some of the most influential and widely adopted cost-containment strategies:
Preventive care and wellness programs
Investing in preventive care initiatives and wellness programs is a proactive approach to control costs in healthcare. By focusing on early detection, lifestyle management, and health education, preventive care aims to identify and nip health issues in the bud before they grow, ultimately minimizing the need for costly treatments.
Utilization management
Utilization management involves evaluating and controlling the utilization of healthcare services to ensure they are necessary and appropriate. This strategy employs tools like prior authorization, case management, and utilization review to avoid unnecessary procedures or treatments, thereby cutting down on superfluous healthcare expenses.
Telehealth and remote monitoring
Telehealth and remote monitoring technologies offer cost-effective solutions by allowing healthcare providers to offer services remotely. These technologies enable consultations, monitoring, and follow-ups without the need for in-person visits, reducing the burden on physical infrastructure and lowering overall healthcare costs.
Negotiating prices and value-based care
Negotiating prices with healthcare providers and adopting value-based care models that focus on outcomes rather than the volume of services rendered can lead to significant cost savings. Value-based care incentivizes quality care delivery while controlling unnecessary procedures or treatments.
Adopting technology and digital tools
Integrating health information technology (HIT) systems, such as electronic health records (EHRs), can streamline healthcare operations. EHRs enhance efficiency, reduce errors, and improve communication among healthcare professionals, ultimately cutting down on administrative costs and redundant procedures.
Financial and plan design
Employers can take control of rising healthcare costs by using smart financial strategies and plan design tools that align spending with employee needs.
- MERPs (Medical Expense Reimbursement Plans):
MERPs allow employers to reimburse employees for specific medical expenses directly, helping control costs without relying solely on high-premium health plans.
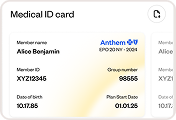
- HRAs and HSAs:
These are tax-advantaged accounts that let employees set aside money for medical expenses, giving them more control over how they spend on care while encouraging cost-conscious choices.
- Reference-Based Pricing (RBP):
RBP is a payment model where employers pay providers based on a set benchmark (like a percentage of Medicare rates) rather than the full billed amount.
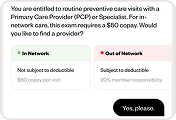
- Tiered Networks:
Tiered networks group providers by cost and quality, offering employees better coverage or lower out-of-pocket costs when they choose high-value, lower-cost providers.
Patient engagement and education
Engaging employees in their own healthcare journey through education and active participation can have a substantial impact on cost containment.
Informed employees are more likely to adhere to treatment plans, make healthier lifestyle choices, and seek timely care. Which then reduces the need for costly interventions.
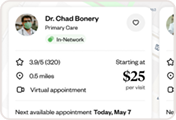
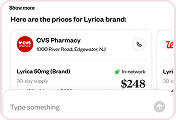
Apps like Healthee can simplify employee healthcare education for employees and companies. With Healthee’s healthcare assistant, employees can now navigate their healthcare options independently and confidently.
The best part is…
They no longer have to wait for endless customer service queues and long back-and-forths with HR just to get their healthcare inquiries answered.
Implementing these strategies tailored to specific healthcare settings can contribute to containing costs while aiming to improve quality of care.
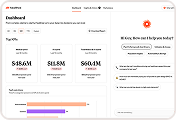
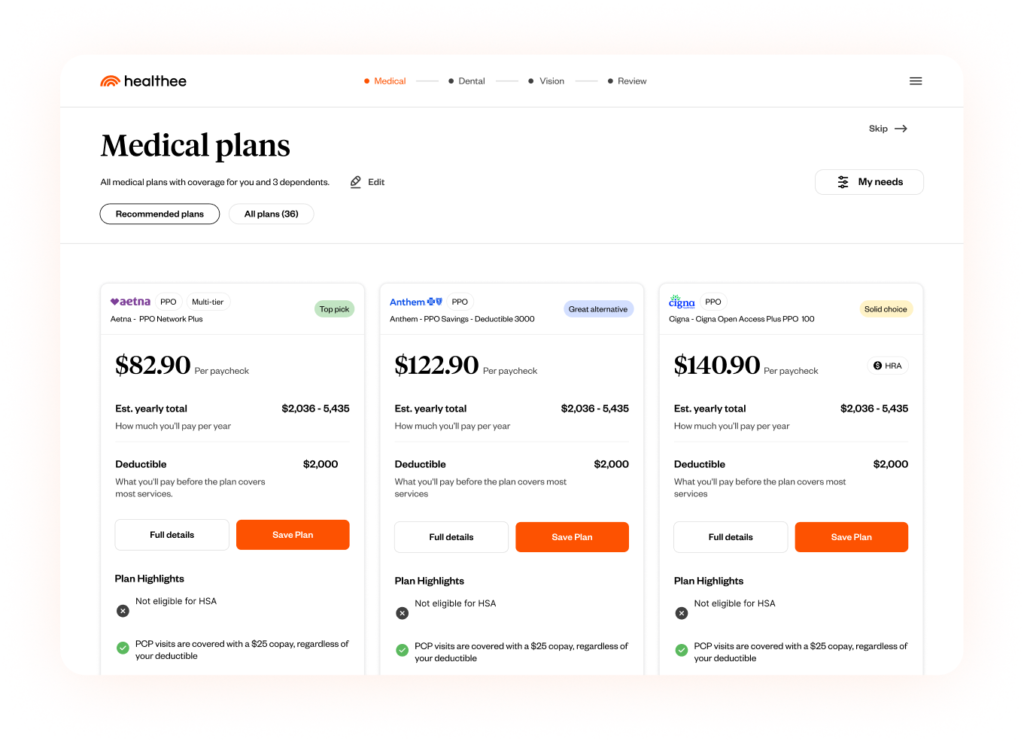
The benefits of Healthee
As healthcare costs skyrocket, cost containment technology is needed more than ever.
Here are a few ways Healthee can help reduce health expenditures while encouraging improved health outcomes.