-
What we do
-
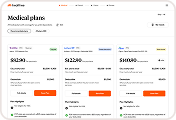
Plan Comparison Tool
AI-powered benefits decision support
-
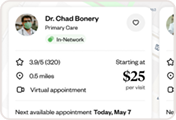
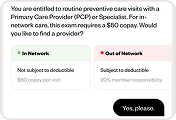
Cost Transparency
Clear cost comparisons for all care
-

Benefits Navigation
Personalized plan exploration
-
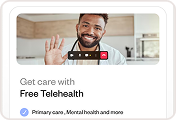
Telehealth
24/7 access to licensed medical care
-
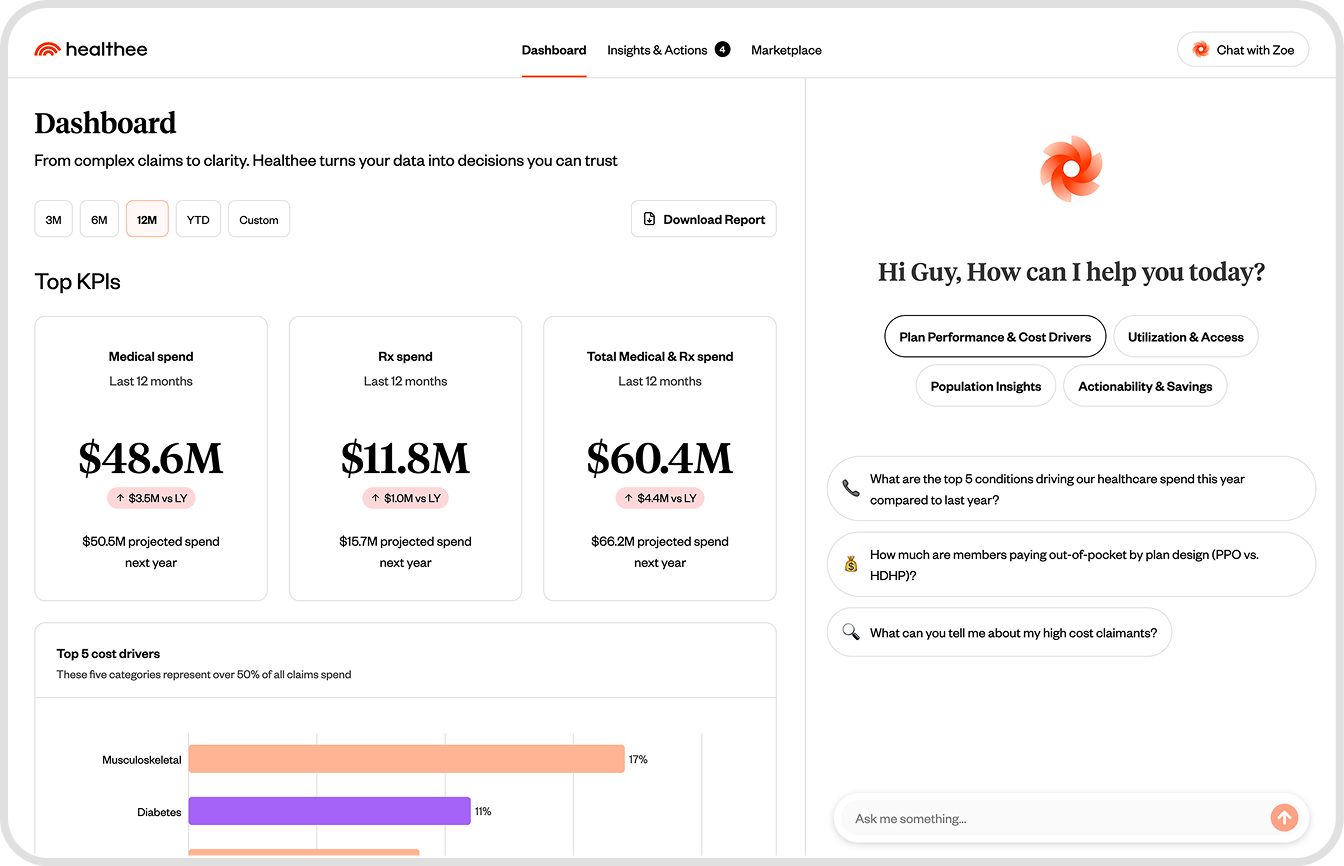
AI Virtual Assistant
Meet Zoe, your personal health agent
-
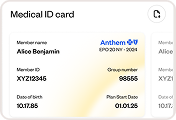
Medical ID
Track deductibles and find your IDs
-
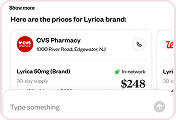
Pharmacy
Unified Rx management and savings
-

Fraud, waste, and abuse
AI FWA engine for recoupment
-
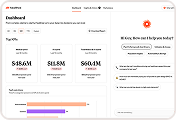
AI claims analytics
Proactive claims intelligence
-

Healthee Access
Custom cash-pay bundled network
-
- Who we serve
- Who we are
-
Resources
-
Contact
Talk to a Healthee Expert