By Dovi Frances, Founding Partner, Group 11 & Guy Benjamin, CEO and Co-founder, Healthee
Picture this: An autonomous AI emergency room physician performs a flawless intake, triage, and diagnosis of a patient’s intense knee pain, reducing wait time by 30%. The patient ends up needing surgery to repair a few tendons, and the procedure goes off without a hitch.
The patient goes home. They’re thrilled with this seamless AI-influenced ER experience …
Then, the $37,000 bill arrives in the mail.
The surgeon was out of network and nobody told them.
Their health plan has a 0% coinsurance policy for out-of-network care.
All the costs fall on them with no help in sight.
And the next eight months become a brutal battle to avoid medical debt.
This is the future we’re racing toward, not because AI failed clinically, but because the system around it stayed exactly the same. The market is being rebuilt by founders who have exciting innovation in mind. But we’re only rebuilding part of the structure while the foundation crumbles beneath us.
The ambitious 8VC whitepaper on AI healthcare regulation maps out a world where artificial intelligence can diagnose, treat, and even bill for medical services.1 It’s an impressive vision, and one that we should strive toward with every AI tool at our disposal.
But we don’t think it’s enough on its own. 8VC’s proposal operates with the core assumption that patients can navigate our byzantine healthcare system well enough to reach these AI providers in the first place.
Here’s the uncomfortable truth that regulatory reformers and policymakers don’t want to (or frankly, aren’t interested to) admit: We could implement every single one of 8VC’s promising AI clinical reforms tomorrow, and it wouldn’t save the patients and their plan sponsors a dime if people keep showing up at the wrong facilities and choosing the wrong plans.
We should dream big — Healthcare AI starts long before the exam room
The 8VC roadmap meticulously outlines three levels of clinical AI integration. They want value-based payment models, federal regulatory frameworks, and eventually, AI systems recognized as reimbursable providers. That’s great. Necessary. Visionary, even.
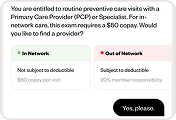
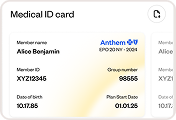
But let’s continue our earlier ER patient story. That same person with the $37,000 surprise bill? Before they ever reached that AI-powered emergency room, they made a good-faith effort to figure out whether the hospital was in-network. But their employer’s benefits portal was down. The insurance company’s phone line had a 75-minute wait. The hospital’s website only listed insurance documentation from three years ago. But since they were in immense “it’s an emergency” type pain, their judgment was clouded, and they couldn’t wait hours for the right answer. When the patient finally arrived without an insurance answer (in severe pain, no less), they had no idea what kind of financial nightmare they were walking into — one that all the clinical AI brilliance in the world couldn’t prevent.
We all know this isn’t a hypothetical or edge case. It’s a regular Tuesday morning in American healthcare.

AI at the beginning of the care journey
For benefits leaders reading this, you’re nodding because you field these calls every week. Your people are making healthcare decisions in information vacuums, then suffering the financial consequences. A recent study by McKinsey found that AI has the potential to save $265 billion in overall healthcare costs by eliminating administrative overhead and documentation errors.2
Yet this study and our entire regulatory conversation are focused on what happens inside the exam room, not the chaos before a patient walks in the door and the months after. We’re compressing time in clinical moments with AI while expanding it everywhere else. This selective optimization ignores where the real hemorrhaging happens.
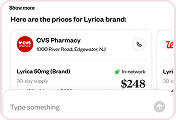
Think about the tragic irony here: We’re building AI sophisticated enough to perform differential diagnoses, but employees still can’t get a straight answer about whether their child’s physical therapy is covered. Again, we’re teaching machines to interpret MRIs (sometimes catching what seasoned doctors aren’t) while people can’t interpret their own Summary of Benefits and Coverage (SBC) spreadsheet.
The tech-forward medical centers implementing cutting-edge clinical AI? They’re operating like five-star restaurants hidden in unmarked buildings with no address. The best healthcare in the world doesn’t matter if employees can’t find it, afford it, or get reimbursed for it.
AI-supported care after the exam
Let’s finish our ER patient’s journey. After eight months of fighting that $37,000 bill, emailing and calling the hospital, explaining their limited resources, and applying for financial assistance, they finally got it reduced to $12,000. Still a crushing bill, but possibly survivable.
Are we okay calling this “success”? We know we’re not. Medical debt is not merely a financial outcome. It’s the story of systemic failure that no amount of clinical AI can fix alone. In fact, it’s a story of over $220 billion in accumulated medical debt held by Americans 3
This person has no doubt developed anxiety about seeking medical care. Awful benefits navigation has poisoned their relationship with their doctors and even their employer’s HR team who gave them said benefits.
And here’s what makes us so confused: The 8VC vision ends when the patient leaves the exam room, right when the real healthcare nightmare begins. Why do we want to add autonomous AI providers to this mix without first fixing the navigation and billing infrastructure? Should 8VC’s technological revolution happen and AI physicians start seeing patients — imagine the administrative chaos when people start receiving bills from AI providers that insurance companies aren’t ready to recognize as legitimate entities.
“Sorry, our system doesn’t have a code for ‘autonomous AI physician.’ You’ll need to pay out of pocket and submit for reimbursement.” Good luck explaining those claims to your people.
The trillion-dollar arbitrage opportunity
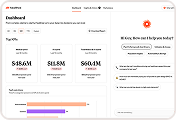
Let’s talk numbers that catch VCs’ attention. The gap between clinical AI innovation and navigation infrastructure is the largest arbitrage opportunity in modern healthcare.
We have $4.5 trillion in annual U.S. healthcare spending, with roughly $265 billion wasted on administrative complexity alone. The 8VC reforms address maybe 20% of that opportunity. The other 80%? That’s where forward-thinking founders, investors, insurance advisors, HR leaders, government policymakers, and physicians themselves should be looking.
We see the market dynamics first-hand: Every Fortune 500 company we’ve spoken with is telling us they’re desperate to control healthcare costs. They explain how benefits navigation is complexifying at the same time plan utilization is bottoming out. They’re waiting for something more than small point solutions that nibble at the margins. The first platform to solve this comprehensively doesn’t just win a market; it defines an entirely new category.
From a regulatory perspective, navigation AI faces far fewer barriers than clinical AI. It’s a (relatively) easy win that has an incredible impact from day one. This is a rare moment where regulation won’t hinder innovation, not the other way around. But the window won’t stay open forever.

The coalition we actually need
The 8VC authors call for a concerted effort to pass legislation on AI in the exam room. But where is the coalition that wants to fix how much Americans navigate and pay for healthcare?
According to KFF, employers cover about 83% of family health insurance premiums and 73% of single coverage premiums.4 These plan sponsors aren’t bystanders. They’re the primary funders of the system we’re trying to reform.
Where are the benefit advisors who want to use AI to translate this complex system for millions of Americans? Where are the HR leaders who want to rely on AI to support employee benefits confusion? Where are the providers who want patients to have clear, tech-enabled navigation before they get to their practice door?
This coalition is splintered, just like the healthcare system at large. And that’s exactly why our ER patient from earlier will still be drowning in medical debt despite receiving care from the most advanced AI physicians in the world.
Building an effective coalition requires institutional pipelines: academia teaching it, policymakers enabling it, and enterprises deploying it at scale. AI cannot be a fractured tool spread across a fractured healthcare system. Healthcare navigation needs the same coordinated, multi-stakeholder approach.
Four points for expanding the vision of AI healthcare reform:
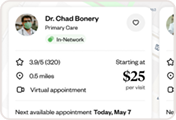
- Navigation before diagnosis: Before we authorize AI to diagnose, let’s use it to navigate. Create reliable AI-powered benefits guidance that steers employees to the right care at the best price.
- Administrative efficiency: Any regulation recognizing clinical AI must simultaneously recognize administrative AI. If an AI can prescribe medication, it must be able to verify insurance coverage and prevent billing errors, too.
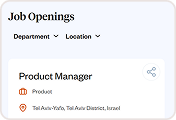
- Employer integration: Include employer-sponsored health plans in every regulatory discussion. The roughly 160 million Americans with employer coverage are the silent majority.
- Public sector adoption: Government entities that are drafting the rules and regs are also employers themselves, offering benefits to huge swaths of the nation. Public sector entities must also begin adopting AI navigation for healthcare to realize this ROI for themselves and lead by example.
The sovereign AI race nobody’s watching
The U.S. has the opportunity to expand 8VC’s vision to an all-encompassing vision for sovereign AI healthcare systems. While we’re racing to deliver better healthcare experiences with AI, we must also consider the regulatory opportunities here. We can use this moment to determine which nation masters full-stack healthcare AI first.
Other AI-enabled nations like China and Singapore aren’t just building AI doctors like 8VC envisions. They’re building integrated super-apps with AI at the core. Don’t believe me? Check out WeDoctor, Ping An Good Doctor, and Endeavour AI.
When you take a closer look, China and Singapore aren’t letting these AI ecosystems evolve on their own. They’re taking practical policymaking steps and creating legislation to achieve their goals. China’s New Generation Artificial Intelligence Development Plan (2017) explicitly sets a goal of global AI leadership by 2030, with healthcare listed as one of five priority application areas for developing a core Chinese AI industry value of $140 billion.5 Additionally, China has enacted multiple regulations that enable AI development, including the Interim Measures for the Administration of Generative AI Services, the Guiding Principles for Classification and Definition of AI Medical Software Products, and the Reference Guidelines for AI Scenarios in Healthcare.6
Singapore has taken an equally aggressive but more targeted approach. Their AI in Healthcare Guidelines (AIHGle), published in 2021 by the Ministry of Health, provides comprehensive recommendations for safe AI development and implementation across clinical environments.7 Beyond regulatory commitments, Singapore is funneling massive capital into AI development. The country has committed over S$500 million through AI Singapore (AISG) under their Research, Innovation and Enterprise (RIE) plans, with a new commitment of more than $1 billion over five years for their National AI Strategy 2.0.
In the face of such advancements and commitments, the U.S. risks winning the AI research race while losing the implementation war.
Healthcare efficiency is economic competitiveness. Every dollar wasted on administrative complexity is a dollar not invested in R&D, education, or infrastructure … or, better yet, savings back in the pocket of patients. Every hour employees spend fighting insurance claims is an hour of lost productivity. In fact, an American Academy of Physician Associates (AAPA) and Harris Poll survey found that Americans waste eight hours coordinating healthcare each month, including scheduling appointments and navigating billing and insurance payments.8 With an estimated 20 million Americans owing medical debt and trying to fight it, that quickly turns into 1.9 billion wasted hours navigating the health system.2 At the scale of our entire U.S. economy, AI healthcare solutions can fix this GDP problem.
The financial implications cascade through markets: Companies with better healthcare navigation see higher employee retention,9 fewer sick days,10 and fewer hours lost to employees fighting medical bills during office hours.11
The first country to solve healthcare navigation at scale — and we believe this must include AI — will unleash its human capital en masse. That’s the real impact of connecting healthcare AI to sovereign AI. We see a U.S. that doesn’t just have the best AI doctors, but has the best AI healthcare navigation journeys from symptom to payment. And even AI that promotes early detection and helps prevent diseases altogether.
It’s time to choose: Partial reform or all-encompassing vision
We stand at a crossroads, and the path we choose will determine whether our ER patient, and all ER patients for that matter, will have the support they need in 2026 and beyond.
Path one: We pursue the 8VC vision in isolation. We create clinical AI marvels that most Americans can’t access, afford, or understand. We build a two-tier system where the healthcare-literate thrive while everyone else drowns in complexity.
Path two: We expand the AI in healthcare vision. We recognize that healthcare goes far beyond the exam room to the entire journey from feeling sick to final payment. We build AI that guides patients to the right care, ensures proper coverage, and prevents billing disasters.
For healthcare and benefits leaders, the choice is obvious. Your people probably couldn’t care less about robot doctors. They’re begging for help with the basics: finding in-network providers, understanding plan coverage, and avoiding financial ruin from medical bills. Let’s avoid just adding expensive technology to a broken system.
The real revolution in AI healthcare won’t come from autonomous physicians. It will come when that ER patient can walk into any medical facility, confident they’ll receive the proper care at a transparent price with no surprises.
About the authors
Guy Benjamin is CEO and Co-founder of Healthee, which provides AI-powered health and benefits navigation to over 1 million households.
Dovi Frances is an Israeli-American venture capitalist and the Founding Partner of Group 11, a Los-Angeles-based VC firm investing in visionary entrepreneurs using the unstoppable momentum of technology and AI to reshape industries. Frances is also a Co-founder of The Institute-Israel’s AI Advancement Center.
About Healthee
Healthee is a leading company in the health tech industry, focused on transforming how employees navigate healthcare and benefits. With a mission to make access to a healthier life effortless, Healthee utilizes AI technology to simplify complex benefits systems, enhancing user experience, cutting costs, and improving care outcomes. The Healthee platform is designed to make healthcare more accessible, personalized, and efficient. For more information, visit Healthee.com or connect with Healthee on LinkedIn, Instagram, Facebook, X, and YouTube.
For more information, please contact:
Omer Maman
VP of Marketing
Healthee
omer@healthee.com
References
- Sebastian Caliri. “A Vision for Healthcare AI in America.” 8VC, December 3, 2025. https://www.8vc.com/resources/ai-healthcare-vision
- Shameek Rakshit, Matthew Rae Twitter, Gary Claxton, Krutika Amin, and Cynthia Cox. “The burden of medical debt in the United States”. KFF, February 12, 2024. https://www.healthsystemtracker.org/brief/the-burden-of-medical-debt-in-the-united-states
- Nikhil R. Sahni, Prakriti Mishra, Brandon Carrus, and David M. Cutler. “Administrative simplification: How to save a quarter-trillion dollars in US healthcare.” McKinsey & Company, October 20, 2021. https://www.mckinsey.com/industries/healthcare/our-insights/administrative-simplification-how-to-save-a-quarter-trillion-dollars-in-us-healthcare
- “2024 Employer Health Benefits Survey.” KFF, October 9, 2024. https://www.kff.org/health-costs/report/2024-employer-health-benefits-survey/
- Gil Zhang, Diana Li, Muran Sun, and Huihui Li. “Healthcare AI 2025: China.” Chambers and Partners, August 6, 2025. https://practiceguides.chambers.com/practice-guides/healthcare-ai-2025/china/trends-and-developments
- Jia J, Zhao S. Ethical and Legal Governance of Generative AI in Chinese Healthcare. J Multidiscip Healthc. 2025 Sep 1;18:5405-5419. doi: 10.2147/JMDH.S541271. PMID: 40917542; PMCID: PMC12412760. https://pubmed.ncbi.nlm.nih.gov/40917542/
- “Artificial Intelligence in Healthcare Guidelines (AIHGIe).” Singapore Ministry of Health, October 2021. https://isomer-user-content.by.gov.sg/3/9c0db09d-104c-48af-87c9-17e01695c67c/1-0-artificial-in-healthcare-guidelines-(aihgle)_publishedoct21.pdf
- “U.S. Adults Spend Eight Hours Monthly Coordinating Healthcare, Find System ‘Overwhelming.’” American Academy of Physician Associates (AAPA), May 17, 2023. https://www.aapa.org/news-central/2023/05/u-s-adults-spend-eight-hours-monthly-coordinating-healthcare-find-system-overwhelming/
- Paige McGlauflin. “Exclusive: Almost half of employers are planning to give out raises, but what workers really want is better benefits.’ Fortune, January 17, 2024. https://fortune.com/2024/01/17/employers-offer-raises-but-employees-want-better-benefits-nfp-survey-exclusive/
- Yasemin Sim Esmen. “Wellness programs cut sick days, improve productivity.” Employee Benefit News, June 13, 2018. https://www.benefitnews.com/news/wellness-programs-cut-sick-days-improves-productivity
- Alana Semuels. “When Fighting with Your Insurance Company Becomes a Full-Time Job.” Time, May 13, 2025. https://time.com/7284610/fighting-health-insurance-company-denial/